A Patient's Guide to Gout
Introduction
Gout is a disease that involves the build-up of uric acid in the body. About 95 percent of gout patients are men. Most men are over 50 when gout first appears. Women generally don't develop gout until after menopause. But some people develop gout at a young age.
This guide will help you understand
- how gout develops
- which parts of the body are affected by gout
- what can be done for the condition
Anatomy
What is gout?
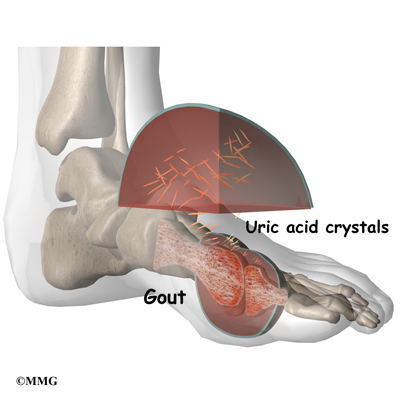
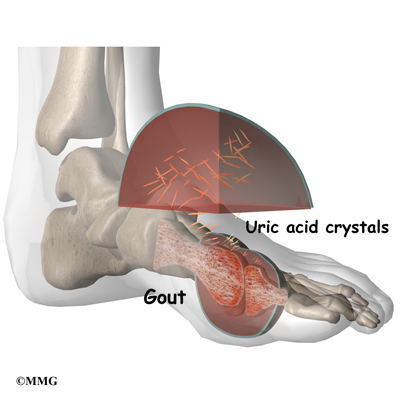
Gout was the first disease in which researchers recognized that crystals in the synovial fluid could be the cause of joint pain. Synovial fluid is the fluid that the body produces to lubricate the joints. In gout, excess uric acid causes needle-shaped crystals to form in the synovial fluid. Uric acid is a normal chemical in the blood that comes from the breakdown of other chemicals in the body tissues.
Everyone has some uric acid in his blood. As your immune system tries to get rid of the crystals, inflammation develops. For the person with too much uric acid, this inflammation can cause painful arthritis.
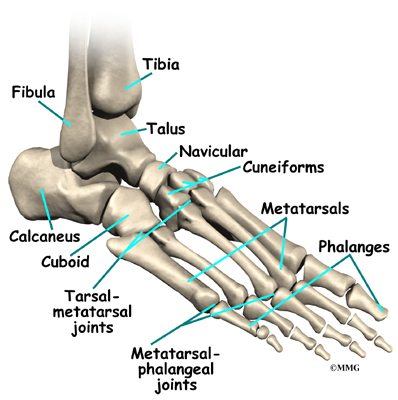
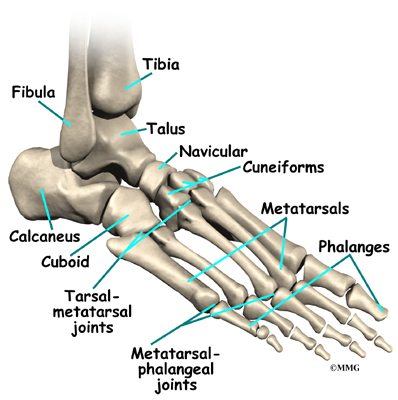
The first attack of gouty arthritis usually happens in just one joint. Half of the time, gout affects the metatarsophalangeal (MTP) joint. This is the joint at the base of the big toe. Eventually, 90 percent of people with gout will have pain in the MTP joint. Other joints that are commonly affected include the mid-foot, ankle, heel, and knee joints. Less commonly gout affects the fingers, wrists, and elbows.
Over time, patients with gout can develop tophi, or lumps that grow around crystal deposits in joints or near pressure points. Tophi most often occur in the fingers, wrists, ears, knees, elbows, forearms, and heels. Tophi can also grow in the kidneys, heart, and eyes.
Causes
Why does gout develop?
Hyperuricemia
The underlying condition that causes gout is called hyperuricemia. It means that you have high levels of uric acid in your blood. This can happen for two reasons: (1) your body creates too much uric acid, or (2) your kidneys don't excrete the uric acid effectively. Whether or not you will develop gout is related to how bad your hyperuricemia is over time.
For people who create too much uric acid, the cause is usually genetic. Some rare genetic and metabolic disorders can cause overproduction of uric acid, which can eventually lead to gout. The breakdown of purines in the body also releases uric acid. Purines are ingested through certain types of food such as sweetmeats (e.g., liver, kidney, brain) and seafood. The increased intake of fructose-sweetened soft drinks has also been linked with an increased risk of gout. Usually the excess uric acid is then passed out of the body through the urine.
More than 90 percent of people with gout have kidneys that don't effectively get rid of uric acid. Sometimes this is caused by certain kinds of drugs, such as diuretics, cyclosporine, and low-dose aspirin. Other medical conditions, such as obesity, hypertension, and diabetes, can also make some people more likely to develop gout.
Many gout patients have a combination of overproduction and under-excretion of uric acid. Their bodies create too much uric acid and have problems getting rid of it. This combination of problems happens with drinking alcohol, especially beer. The more alcohol the patient drinks, the worse the problem is. Alcohol both raises uric acid levels in the body and impairs the kidneys' ability to excrete the buildup.
Acute Causes
Attacks of gouty arthritis seem to be caused by sudden increases in the amount of urate (a solid form of uric acid) in your synovial fluid. This rapid change can be caused by injury to the joint, alcohol use, or use of certain drugs.
An injury that can trigger gout can be very slight. Even gentle exercise can cause inflammation in the joint, although you may not notice it. Once the joint is at rest, the body absorbs some of the water in the synovial fluid. This leaves the synovial fluid more concentrated with urate, which may allow crystals to grow.
Other Factors
Heredity plays a role in gout. In some families, hyperuricemia tends to develop into gout, while in other families it doesn't. But genes alone don't account for gout. The rising number of people with gout since World War II suggests more than just a genetic or hereditary basis for this condition.
Dietary changes may be the major difference over the last 60 years. Food scarcity during the 1940s was followed by an increased intake of carbohydrates and especially carbohydrates containing high-fructose corn syrup. The increase in obesity (another risk factor for gout) during the same time supports this idea.
There are several other risk factors for gout. These conditions do not cause gout, but they are closely related to severe hyperuricemia. The risk factors include metabolic syndrome, kidney problems, high hemoglobin levels, high triglyceride levels, and hypertension (high blood pressure). About 14 percent of hypertension patients have gout. A combination of factors such as eating lots of organ meat, a sedentary lifestyle without exercise, and drinking lots of alcohol increases the risk for symptomatic gout.
It is important to note that hyperuricemia alone doesn't cause gout. Most people with high levels of uric acid in their blood never develop any symptoms of gout. At least five percent of Americans have at least one period of hyperuricemia as adults without showing any symptoms of gout. And most people can tolerate fairly high levels of uric acid in their bloodstream without damage to their kidneys.
Symptoms
What does gout feel like?
Gout causes attacks of very painful joint inflammation. This pain is often described as burning pain. Early gout attacks usually affect only one joint. This joint is most commonly the MTP joint at the base of your big toe. The joint becomes swollen, warm, and red within eight to 12 hours. Most of the time the attacks happen at night. Patients say the pain is so bad the joint can't even stand the slightest touch. Even the weight of a sheet causes excruciating pain. Walking and standing are almost impossible if the legs or feet are affected. Many patients have flu-like symptoms, including fever and chills. The pain may go away on its own in a few hours, or it may take a few weeks.
Gouty arthritis attacks come and go. There may be months between attacks. Over time the attacks happen more often, last longer, and involve more joints. Eventually the pain doesn't ever completely go away. The joints stay swollen and tender even between flare-ups, and the flare-ups start to happen every few weeks. Eventually, some patients develop tophi on joints or pressure points and kidney stones.
Diagnosis
How do doctors identify the condition?
Diagnosis is important because crystals within the joint can lead to joint damage. This can happen without you knowing it. Patients with arthritic episodes that come and go may not seek medical help. Some patients are medically evaluated but complete testing is not done. They are misdiagnosed with rheumatoid arthritis. Either of these situations will delay treatment and increase the risk of erosive damage to the joint.
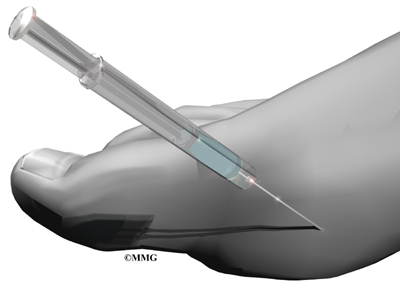
The diagnosis begins with a history of your symptoms and a physical exam. Your doctor will need to look at synovial fluid from the affected joint to identify the needle-like crystals. This is the most important part of the diagnosis. To get a sample of the synovial fluid, the physician performs an arthrocentesis. A long, thin needle is inserted into the affected joint and a small amount of synovial fluid is aspirated or removed. The fluid is sent to a laboratory where it is viewed under a special polarized light microscope to determine if uric acid crystals are present.
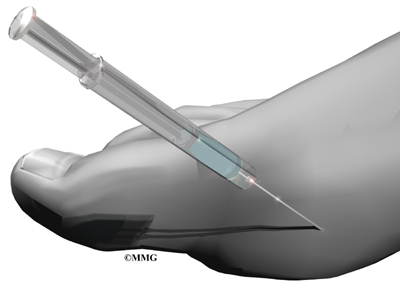
If there are uric acid crystals, then you have gout. But only 80 per cent of the tests are positive when the person really has gout, so this test is not completely accurate. In some cases (such as the midfoot), it isn't easy to aspirate fluid. Without the use of fluoroscopy (a special X-ray imaging) or ultrasound to guide the needle, aspiration isn't done. In these situations, the diagnosis is made without joint aspiration when the patient responds favorably to therapy.
Musculoskeletal ultrasonography (MSUS) is another imaging method used to evaluate gouty joints. This noninvasive technique shows where the crystals have been deposited in the joint. Ultrasound pictures show the hyaline cartilage -- the cartilage that coats the ends of the bones to protect them.
The diagnosis must rule out the presence of infection, which can be a hidden problem. Your doctor may also get a blood test to look at the levels of uric acid. However, uric acid levels rise and fall depending on many complex factors in your body. It is possible to have a normal uric acid level while you are having severe gout pain.
If you have tophi, your doctor may want to biopsy one of the lumps.
Your doctor will need to rule out other forms of arthritis. Gout can occur with other forms of arthritis, such as septic arthritis and rheumatoid arthritis. There are also other diseases that cause different kinds of crystals to form in the synovial fluid.
X-rays don't show doctors much in the early stages of gout. X-rays can help monitor your disease, and they may be needed to rule out other problems.
Treatment
What can be done for the condition?
Gout cannot be cured, but it can be very successfully treated. The main goal of treating gout is to reduce the amount of urate in your blood. Joint crystals will not dissolve or go away unless the serum urate concentration is below six mg/dL.
During the acute or early phase of a gouty attack, doctors prescribe medicines called colchicine, certain nonsteroidal anti-inflammatory drugs (NSAIDs), and corticosteroids to decrease swelling and relieve pain. All of these drugs work quickly and are very effective. The sooner they are given after an attack starts, the faster the pain goes away. These drugs may be given by mouth, through an intravenous line into your bloodstream, or injected directly into the joint. There are some potential adverse side effects of these medications. It may take a bit of time to find the most effective drug with the least intolerable side effects for some patients. But it is important to start treatment during the first few days of an attack to get the best results.
Your doctor may also decompress the affected joint. Aspiration of synovial fluid immediately decreases the pressure in the joint. And the needle leaves a pathway or track that acts as a vent for continued drainage after the needle is removed.
Lifestyle changes can help you manage intermittent gout without using drugs every day. Your doctor may ask you to do the following:
- Change your diet. Diets that are lower in meat, shellfish, and some other foods can help decrease the amount of uric acid in your body. Avoid fructose sweetened foods and beverages.
- Quit taking drugs such as diuretics.
- Lose weight.
- Quit drinking alcohol.
- Avoid activities that stress your joints.
- Drink plenty of fluids to help your kidneys work more efficiently.
If your gout is severe, prolonged, or chronic, you may need to take daily serum uric acid-lowering (SUA) medication to reduce your uric acid levels. Your doctor will put you on the lowest dose possible of medications such as uricosuric drugs or xanthine oxidase inhibitors. Doctors usually prescribe allopurinol (Zyloprim, a xanthine oxidase inhibitor) for patients who overproduce urates or have tophi, kidney disease, or kidney stones. Allopurinol is useful in preventing recurrence of gouty attacks. It blocks the production of uric acid and decreases the formation of purine. For patients who have difficulty getting rid of uric acid through the kidneys, medications to help the kidneys remove more uric acid from the blood may be prescribed as well. Probenecid is one of the commonly prescribed drugs that increase the removal of uric acid in the urine.
Another, serum uric acid-lowering (SUA) medications that has been shown to reduce the risk of occurrence is Uloric (Febuxostat). Febuxostat has been approved by the FDA for patients with mild to moderate kidney disease. It lowers uric acid slowly enough to avoid flaring up the gout. It isn't processed by the kidney, so it's possible patients with kidney disease may be able to take it. But it is metabolized by the liver. Anyone with a liver problem or who abuses alcohol may not be able to take this drug.
As with all medications, you should report any side effects to your doctor right away. Watch for skin rashes, itching, fever, nausea, vomiting, diarrhea, or other new symptoms not present before taking the serum uric acid medications.
Sometimes patients experience a flare-up after taking urate-lowering agents. This reaction can come as a surprise, since you expect your pain and swelling to get better. Flares of this kind mean that old deposits of crystals stored in the tissues are being released. The increase in symptoms is not a sign that new crystals are forming. Don't stop taking your medication without first checking with your doctor. Getting rid of the old crystals can help protect the joint from further damage.
Doctors seldom treat hyperuricemia without symptoms of gout. However, if hyperuricemia is at least moderately bad over several years, it is more likely to lead to gout. In this case, a doctor may begin treatments to prevent gout. This is called prophylaxis.
A program to control uric acid levels and manage symptoms often includes daily colchicine and allopurinol or probenecid (usually both are not taken at the same time) along with dietary restrictions. Regular follow-up with your physician and blood tests to detect serum uric acid concentration that are above the six mg/dL target level are important in maintaining good control and preventing joint erosion.
What's new on the market for the pharmaceutical (drug) treatment of gout? New understanding of the exact mechanisms behind gout has led to the development of new agents for patients with refractory gout. Refractory means the symptoms won't go away and the condition has become chronic and unmanageable.
These new treatments called uricase therapy aren't available for use in the general public. They are just in the experimental stages. Drug companies are looking to find ways to use enzymes that convert uric acid into an acid that will be readily absorbed and passed out of the body. One of these enzymes is uricase. Humans don't have this enzyme naturally but other animals do. The use of pig and baboon uricase called pegloticase therapy is under investigation and pending FDA approval.
Some researchers are using medications already on the market but used for other problems. This practice is referred to as off-label use. One drug in particular (rasburicase) normally used to break down cancerous tumors has been tested. It seems to work but it is very expensive so that won't work if a patient is supposed to take it for a long time.
Right now uricase (biologic) therapy is an induction therapy, which means it is administered intravenously. Infusion reactions are holding things back a bit. At least 10 per cent of the patients receiving induction therapy experience severe adverse reactions including flushing, hives, low blood pressure, chest pain, and muscle cramping. It may be possible eventually to start with an intravenous dose, get the symptoms under control, and then switch to a pill form of the same medication to maintain results.
The future looks promising for gout sufferers. It seems certain that better understanding of purine metabolism will come to light in the very near future. Experts feel sure that it's only a matter of time before scientists hit upon a pharmaceutical "cure" for cases of gout that can't be managed otherwise with diet and exercise.
|