A Patient's Guide to Shoulder Instability
Introduction
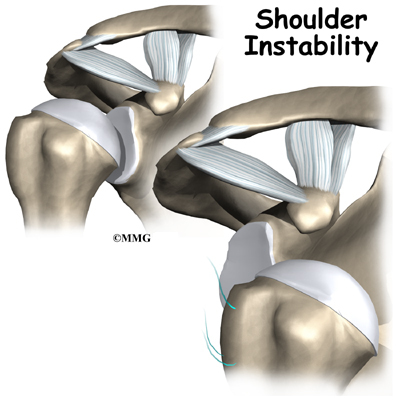
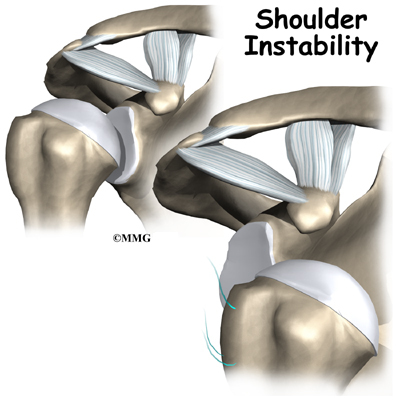
Shoulder instability means that the shoulder joint is too loose and is able to slide around too much in the socket. In some cases, the unstable shoulder actually slips out of the socket. If the shoulder slips completely out of the socket, it has become dislocated. If not treated, instability can lead to arthritis of the shoulder joint.
This guide will help you understand
- what parts of the shoulder are involved
- what causes shoulder instability
- what treatments are available
Anatomy
What parts of the shoulder are involved?
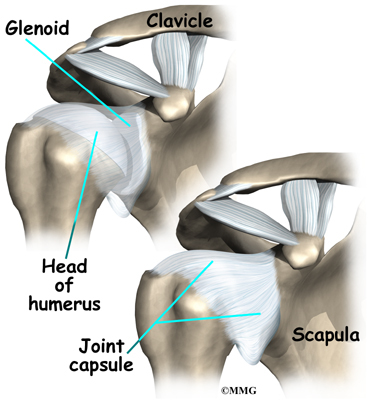
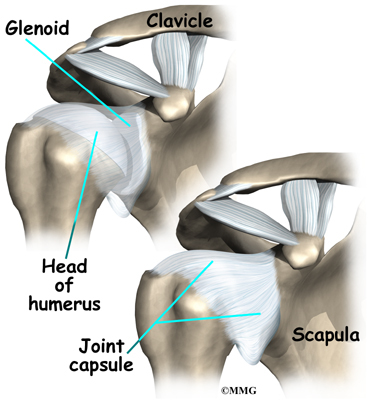
The shoulder is made up of three bones: the scapula (shoulder blade), the humerus (upper arm bone,) and the clavicle (collarbone).
The rotator cuffconnects the humerus to the scapula. The rotator cuff is actually made up of the tendons of four muscles: the supraspinatus, infraspinatus, teres minor, and subscapularis.
Tendons attach muscles to bones. Muscles move bones by pulling on tendons. The muscles of the rotator cuff also keep the humerus tightly in the socket. A part of the scapula, called the glenoid, makes up the socket of the shoulder. The glenoid is very shallow and flat. A rim of soft tissue, called the labrum, surrounds the edge of the glenoid, making the socket more like a cup. The labrum turns the flat surface of the glenoid into a deeper socket that molds to fit the head of the humerus.
Surrounding the shoulder joint is a watertight sac called the joint capsule. The joint capsule holds fluids that lubricate the joint. The walls of the joint capsule are made up of ligaments. Ligaments are soft connective tissues that attach bones to bones. The joint capsule has a considerable amount of slack, loose tissue, so that the shoulder is unrestricted as it moves through its large range of motion. If the shoulder moves too far, the ligaments become tight and stop any further motion, sort of like a dog coming to the end of its leash.
Dislocations happen when a force overcomes the strength of the rotator cuff muscles and the ligaments of the shoulder. Nearly all dislocations are anterior dislocations, meaning that the humerus slips out of the front of the glenoid. Only three percent of dislocations are posterior dislocations, or out the back.
Sometimes the shoulder does not come completely out of the socket. It slips only partially out and then returns to its normal position. This is called subluxation.
Related Document: A Patient's Guide to Shoulder Anatomy
Causes
What makes a shoulder become unstable?
Shoulder instability often follows an injury that caused the shoulder to dislocate. This initial injury is usually fairly significant, and the shoulder must be reduced. To reduce a shoulder means it must be manually put back into the socket. The shoulder may seem to return to normal, but the joint often remains unstable. The ligaments that hold the shoulder in the socket, along with the labrum (the cartilage rim around the glenoid), may have become stretched or torn. This makes them too loose to keep the shoulder in the socket when it moves in certain positions. An unstable shoulder can result in repeated episodes of dislocation, even during normal activities. Instability can also follow less severe shoulder injuries.
Related Document: A Patient's Guide to Labral Tears
In some cases, shoulder instability can happen without a previous dislocation. People who do repeated shoulder motions may gradually stretch out the joint capsule. This is especially common in athletes such as baseball pitchers, volleyball players, and swimmers. If the joint capsule gets stretched out and the shoulder muscles become weak, the ball of the humerus begins to slip around too much within the shoulder. Eventually this can cause irritation and pain in the shoulder.
A genetic problem with the connective tissues of the body can lead to ligaments that are too elastic. When ligaments stretch too easily, they may not be able to hold the joints in place. All the joints of the body may be too loose. Some joints, such as the shoulder, may be easily dislocated. People with this condition are sometimes referred to as double-jointed.
Symptoms
What problems does an unstable shoulder cause?
Chronic instability causes several symptoms. Frequent subluxation is one. In subluxation, the shoulder may slip (sublux) in certain positions, and the shoulder may actually feel loose. This commonly happens when the hand is raised above the head, for example while throwing. Subluxation of the shoulder usually causes a quick feeling of pain, like something is slipping or pinching in the shoulder. Over time, you may stop using the shoulder in ways that cause subluxation.
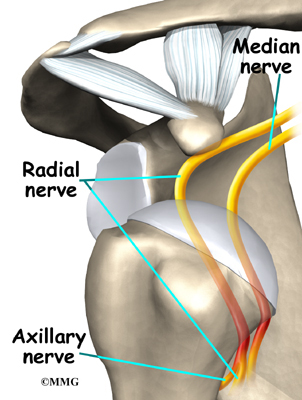
The shoulder may become so loose that it starts to dislocate frequently. This can be a real problem, especially if you can't get it back in the socket and must go to the emergency room every time. A shoulder dislocation is usually very obvious. The injury is very painful, and the shoulder looks abnormal. Any attempted shoulder movements cause extreme pain. A dislocated shoulder can damage the nerves around the shoulder joint.
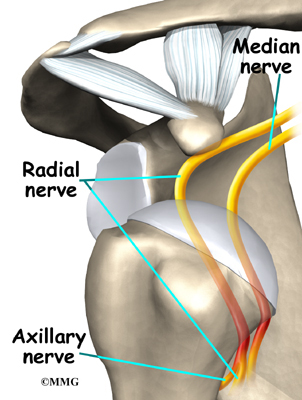
If the nerves have been stretched, a numb spot may develop on the outside of the arm, just below the top point of the shoulder. Several of the shoulder muscles may become slightly weak until the nerve recovers. But the weakness is usually temporary.
Related Document: [relateddocument id=""]A Patient's Guide to Shoulder Dislocations[/relateddocument]
Diagnosis
What tests will my doctor run?
Your doctor will diagnose shoulder instability primarily through your medical history and physical exam. The medical history will include many questions about past shoulder injuries, your pain, and the ways your symptoms are affecting your activities.
In the physical exam, your doctor will feel and move your shoulder, checking it for strength and mobility. Your doctor will stress the shoulder to test the ligaments. When the shoulder is stretched in certain directions, you may get the feeling that the shoulder is going to dislocate. This is a very important sign of instability. It is called an apprehension sign. (Don't worry. Unless your shoulder is extremely loose, it will not dislocate.)
Your doctor may order an X-ray. X-rays can help confirm that your shoulder was dislocated or injured in the past.
If your doctor is unsure about the diagnosis, you may need to undergo further tests. A surgeon may need to examine your shoulder using an arthroscope while you are under general anesthesia, which puts you to sleep. An arthroscope is a tiny TV camera inserted into the shoulder through a small incision. This allows a good look at the muscles and ligaments of the shoulder. When you are awake, it is hard to test the ligaments because you automatically tighten the muscles during the exam.
When you go to the doctor with a dislocated shoulder, X-rays are necessary to rule out a fracture. X-rays are usually done after the shoulder is put back into joint. This allows your doctor to make sure the joint is back in place.
Treatment
What treatment options are available?
Nonsurgical Treatment
Your doctor's first goal will be to help you control your pain and inflammation. Initial treatment to control pain is usually rest and anti-inflammatory medication, such as aspirin or ibuprofen. Your doctor may suggest a cortisone injection if you have trouble getting your pain under control. Cortisone is a strong anti-inflammatory medication.
Your doctor will probably have a physical or occupational therapist direct your rehabilitation program. At first, patients are shown ways to avoid positions and activities that put the shoulder at further risk of injury or dislocation. Overhand athletes may be issued a special shoulder strap or sleeve to stop the shoulder from moving in ways that strain it.
Your therapist may use heat or ice treatments to ease pain and inflammation. Hands-on treatments and various types of exercises are used to improve the range of motion in your shoulder and nearby joints and muscles. Later, you will do strengthening exercises to improve the strength and control of the rotator cuff and shoulder blade muscles. Your therapist will help you retrain these muscles to keep the ball of the humerus in the socket. This will improve the stability of the shoulder and help your shoulder joint move smoothly.
You may need therapy treatments for six to eight weeks. Most patients are able to get back to their activities with full use of their arm within this amount of time.
Surgery
If your therapy program doesn't stabilize your shoulder after a period of time, you may need surgery. There are many different types of shoulder operations that have been developed and used in the past to stabilize the shoulder. Almost all of these operations attempt to tighten the ligaments that are loose. The loose ligaments are usually along the front or bottom part of the shoulder capsule.
Surgery on the shoulder has improved dramatically over the past two decades. many of the procedures that have been developed in the past have been abandoned altogether. Today, surgery that is performed for stabilizing an unstable shoulder is most commonly done using the arthroscope.
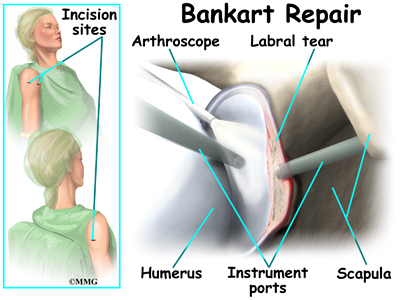
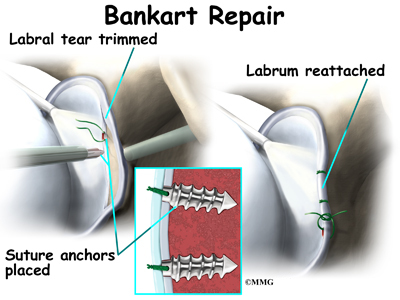
Bankart Repair
The most common method for surgically stabilizing a shoulder that is prone to anterior dislocations is the Bankart repair. In the past, the Bankart repair was done through a large incision made in the front (anterior) shoulder joint. This required damage to a great deal of normal tissue in order for the surgeon to be able to see the damaged portion of the joint capsule. The procedure was difficult and usually involved an attempt to sew or staple the ligaments on the front side of the joint back into their original position.
The arthroscope has changed all that.
An arthroscope is a special type instrument designed to look into a joint, or other space, inside the body. The arthroscope itself is a slender metal tube smaller than a pencil. Inside the metal tube are special strands of glass called fiberoptics. These small strands of glass form a lens that allows one to look into the tube on one end and see what is on the other side - inside the space. This is similar to a microscope or telescope. In the early days of arthroscopy, the surgeon actually looked into one end of the tube. Today, the arthroscope is attached to a small TV camera. The surgeon can watch the TV screen while the arthroscope is moved around in the joint. Using the ability to see inside the joint, the surgeon can then place other instruments into the joint and perform surgery while watching what is happening on the TV screen.
The arthroscope lets the surgeon work in the joint through a very small incision. This may result in less damage to the normal tissues surrounding the joint, leading to faster healing and recovery. If your surgery is done with the arthroscope, you may be able to go home the same day.
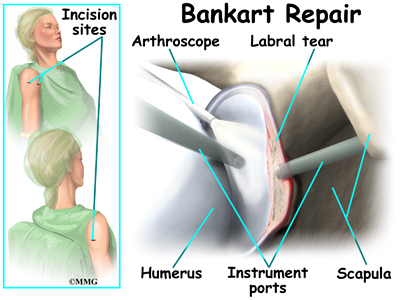
To perform the Bankart type repair using the arthroscope, several small incisions are made to insert the arthroscope and special instruments needed to complete the procedure. These incisions are small, usually about one-quarter inch long. It may be necessary to make three or four incisions around the shoulder to allow the arthroscope to be moved to different locations to see different areas of the shoulder.
A small plastic, or metal, tube is inserted into the shoulder and connected with sterile plastic tubing to a special pump. Another small tube allows the fluid to be removed from the joint. This pump continuously fills the shoulder joint with sterile saline (salt water) fluid. This constant flow of fluid through the joint inflates the joint and washes any blood and debris from the joint as the surgery is performed.
There are many small instruments that have been specially designed to perform surgery in the joint. Some of these instruments are used to remove torn and degenerative tissue. Some of these instruments nibble away bits of tissue and then vacuum them up from out of the joint. Others are designed to burr away bone tissue and vacuum it out of the joint. These instruments are used to remove any bone spurs that are rubbing on the tendons of the shoulder and smooth the under surface of the acromion and AC joint.
Once any degenerative tissue and bone spurs are removed, the torn ligaments that stabilize the shoulder are reattached to the bone around the socket of the shoulder, the glenoid. Special devices have been designed to reattach these ligaments. These devices are called suture anchors.
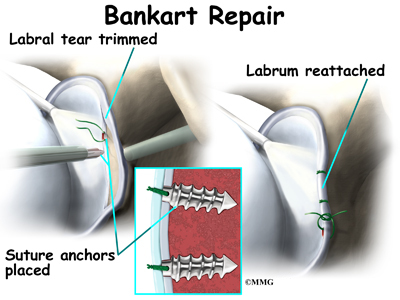
Suture anchors are special devices that have been designed to attach tissue to bone. In the past, many different ways were used to attach soft tissue (such as ligaments and tendons) to bone. The usual methods have included placing stitches through drill holes in the bone, special staples and screws with special washers all designed to hold the tissue against the bone until healing occurred. Most of these techniques required larger incisions to be able to see what was going on and to get the hardware and soft tissue in the right location.
Today, suture anchors have simplified the process and created a much stronger way of attaching soft tissue to bone. These devices are small enough that the can be placed into the appropriate place in the bone through a small incision using the arthroscope. Most of these devices are made of either metal or a special plastic-like material that dissolves over time. This is the anchor portion of the device. The anchor is drilled into the bone where the surgeon wished to attach the soft tissue. Sutures are attached to the anchor and threaded through the soft tissue and tied down against the bone.
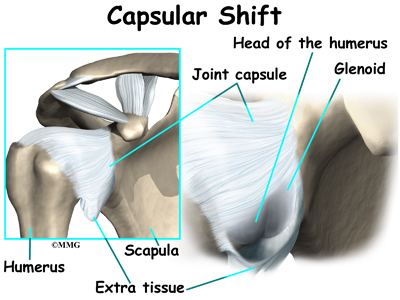
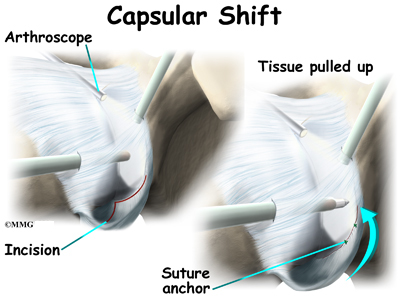
Capsular Shift
Another surgery to tighten a loose shoulder joint is a procedure called a capsular shift. The lining of any joint is called the joint capsule. The joint capsule forms a pocket, or bag that is made up of the ligaments and connective tissue around the joint. The shoulder joint has a fairly large joint capsule that is necessary to allow the joint to move in such a wide range.
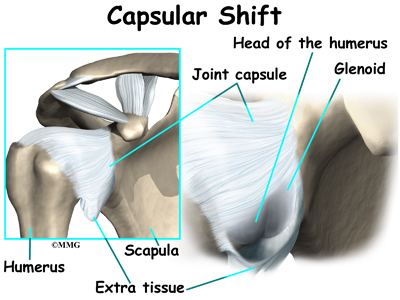
Sometimes the problem causing the shoulder instability is because the joint capsule is simply too large. This is sometimes referred to as a redundant, or patulous joint capsule. This may cause shoulder instability in multiple directions. This is sometimes referred to as multi-directional instability. In order to fix this type of instability, the joint capsule needs to be made smaller and tightened.
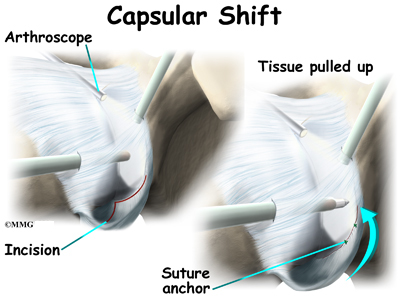
This procedure also can be performed using the arthroscope. The surgeon pulls the flap of tissue over the front of the capsule and connects it together. This is similar to when a tailor tucks loose fabric by overlapping and sewing the two parts together. Once the appropriate degree of tightness is achieved, the surgeon uses a combination of sutures and suture anchors to hold the joint capsule in this position until healing occurs.
Rehabilitation
What should I expect after treatment?
Nonsurgical Rehabilitation
Even nonsurgical treatment for shoulder instability usually requires a rehabilitation program. The goal of therapy will be to strengthen the rotator cuff and shoulder blade muscles to make the shoulder more stable. At first you will do exercises with a therapist. Eventually you will be put on a home program of exercise to keep the muscles strong and flexible. This should help you avoid future problems.
After Surgery
Rehabilitation after surgery is more complex. You will likely wear a sling to support and protect the shoulder for one to four weeks. A physical or occupational therapist may direct your recovery program. Depending on the surgical procedure, you will probably need to attend therapy sessions for two to four months. You should expect full recovery to take up to six months.
The first few therapy treatments will focus on controlling the pain and swelling from surgery. Ice and electrical stimulation treatments may help. Your therapist may also use massage and other types of hands-on treatments to ease muscle spasm and pain.
Therapy after Bankart surgery proceeds slowly. Range-of-motion exercises begin soon after surgery, but therapists are cautious about doing stretches on the front part of the capsule for the first six to eight weeks. The program gradually works into active stretching and strengthening.
Therapy goes even slower after surgeries where the front shoulder muscles have been cut. Exercises begin with passive movements. During passive exercises, your shoulder joint is moved, but your muscles stay relaxed. Your therapist gently moves your joint and gradually stretches your arm. You may be taught how to do passive exercises at home.
Active therapy starts three to four weeks after surgery. You use your own muscle power in active range-of-motion exercises. You may begin with light isometric strengthening exercises. These exercises work the muscles without straining the healing tissues.
At about six weeks you start doing more active strengthening. Exercises focus on improving the strength and control of the rotator cuff muscles and the muscles around the shoulder blade. Your therapist will help you retrain these muscles to keep the ball of the humerus in the socket. This helps your shoulder move smoothly during all your activities.
By about the tenth week, you will start more active strengthening. These exercises focus on improving strength and control of the rotator cuff muscles. Strong rotator cuff muscles help hold the ball of the humerus tightly in the glenoid to improve shoulder stability.
Overhand athletes (such as those who throw baseballs or footballs) start gradually in their sport activity about three months after surgery. They can usually return to competition within four to six months.
Some of the exercises you'll do are designed to get your shoulder working in ways that are similar to your work tasks and sport activities. Your therapist will help you find ways to do your tasks that don't put too much stress on your shoulder. Before your therapy sessions end, your therapist will teach you a number of ways to avoid future problems.
|