A Patient's Guide to Thoracic Outlet Syndrome
Introduction
Thoracic outlet syndrome (TOS) can cause pain and numbness in the shoulder, arm, and hand. Testing for TOS is difficult. There is no one test to accurately diagnose TOS, and other conditions can have similar symptoms. You will need to go through several tests to find out if TOS is actually the cause of your pain. Making the right diagnosis often takes time and can be a cause of frustration, both for you and your doctor.
This guide will help you understand
- what happens to cause TOS
- what tests will be used to diagnose the condition
- what can be done to relieve your pain
Anatomy
What is the thoracic outlet?
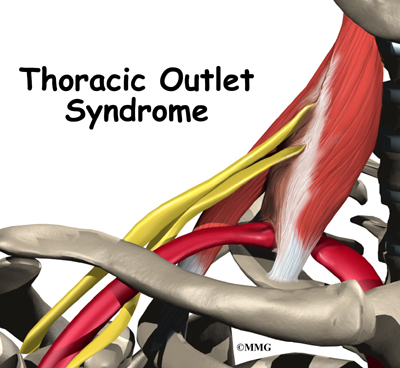
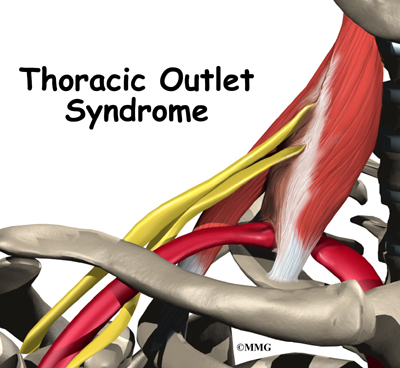
The nerves and blood vessels that go into the arm and hand start at the side of the neck. Nerves come out of the spine through small openings along the side of each vertebra. These openings are called neural foramina.
The nerves and vessels travel between muscles in the neck called the scalene muscles and over the top of the rib cage. The thoracic outlet is this opening between the scalene muscles and the rib cage. The nerves and blood vessels then go under the collarbone (also known as the clavicle), through the armpit (the axilla), and down the arm to the hand.
Related Document: A Patient's Guide to Shoulder Anatomy
Causes
What causes TOS problems?
The main cause of TOS is that the nerves and blood vessels going to the arm and hand get squeezed near the thoracic outlet. This can occur for many reasons.
Pressure on nerves and vessels can happen in people who have fractured their clavicle. It can also happen in people who have an extra first rib, although this doesn't always result in TOS.
Extra muscle or scar tissues in the scalene muscles can put extra pressure on the nerves and arteries. Heavy lifting and carrying can bulk up the scalenus muscles to the point where the nerve and arteries get squeezed.
Traumatic injury from a car accident can also cause problems that lead to TOS. In an accident, the shoulder harness of the seat belt can strain or tear the muscles. As they heal, scar tissue can build up, putting pressure on the nerves and blood vessels at the thoracic outlet.
Neck and arm positions used at work and home may contribute to TOS. People who have to hold their neck and shoulders in awkward alignment sometimes develop TOS symptoms. TOS symptoms are also reported by people who have to hold their arms up or out for long periods of time.
People with TOS often slouch their shoulders, giving them a drooped appearance. The poor body alignment of slouching can compress the nerves and arteries near the thoracic outlet. Being overweight can cause problems with posture, and women who have very large breasts may also have a droopy posture. For some reason, TOS affects three times as many women as men.
Symptoms
What symptoms does TOS cause?
TOS causes pain along the top of the clavicle and shoulder. The pain may spread along the inside edge of the arm. Occasionally pain spreads into the hand, mostly into the ring and pinky fingers. Numbness and tingling, called paresthesia, may accompany the pain, especially in the early hours of the morning before it's time to wake up. Symptoms tend to get worse when driving, lifting, carrying, and writing. The arms may also feel tired when held overhead, as when using a blow dryer. It may be harder to hold and grip things, and the hand may feel clumsy.
Symptoms related to the blood vessels are less common. If the blood vessels are causing symptoms, the arm and shoulder may feel heavy and cold. The arm may become somewhat blue (cyanotic), and the constriction of vessels can cause the arm and hand to swell. Problems with the blood vessels that go to the arm are serious. If you experience these symptoms, you should call your doctor right away.
TOS symptoms are similar to the symptoms of many other conditions. A herniated disc in the neck, carpal tunnel syndrome in the hand, and bursitis of the shoulder can all cause symptoms very much like those of TOS.
Diagnosis
How will my doctor know that I have TOS?
Because TOS doesn't have any unique symptoms, it can be difficult to diagnose. The diagnosis of TOS involves getting as much information as possible to eliminate other possible causes of your pain.
First, your doctor will take your medical history and do a thorough physical examination. Because TOS is so difficult to diagnose, your doctor will rely heavily on what you report about your symptoms and medical history.
You may need to get an X-ray. The X-ray could show an extra cervical rib or other problems with the bones and joints, such as arthritis. Your doctor may also ask you to get an magnetic resonance imaging (MRI) scan or other imaging tests. MRI scans use magnetic waves to show pictures of the bones and soft tissues of your body in slices. X-rays and other imaging tests are mostly used to rule out other problems.
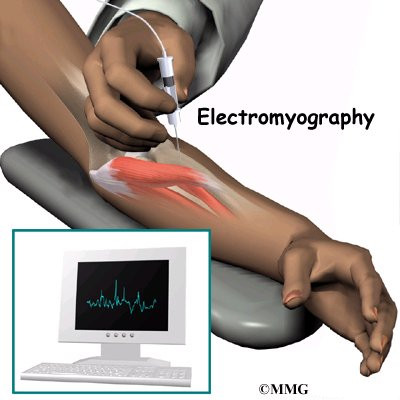
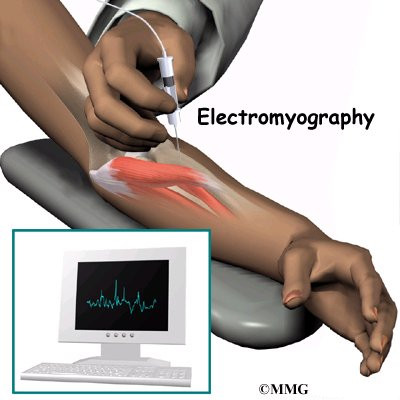
Your doctor may recommend electrical tests, called electromyography, of the nerves in the arm. These tests are used to find out if the nerves between the neck and hand are being pinched.
To confirm the diagnosis, doctors may do special tests of the blood vessels that run along the nerves. These tests are frequently negative, but it is important that your doctor rule out other causes of your pain.
Treatment
What treatment options are available?
Nonsurgical Treatment
Doctors begin treating your pain conservatively, without surgery or other invasive procedures. Your doctor can prescribe some types of medicine to ease your discomfort. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as aspirin and ibuprofen, can relieve pain and inflammation, and muscle relaxants can relieve muscle spasm. Some patients who experience chronic pain, such as the pain of TOS, end up battling depression. In these cases, anti-depressants can be very helpful.
Your doctor may recommend some simple ways to help you combat TOS. For example, decrease the tension of the shoulder strap of your seat belt. Take rest periods to avoid fatigue. Overweight patients should seek help with weight loss, and women with especially large breasts may benefit from using a strapless long-line bra. Avoid heavy lifting, pulling, or pushing. Rapid breathing and stress can worsen symptoms. Avoid looking up, bending the neck back, or holding your arms up for long periods of time. And don't carry a purse or bag on the affected shoulder.
Your doctor may start you on some basic exercises. If you have done them for some time and your symptoms aren't getting much better, you may need to work with a physical or occupational therapist.
In most cases therapy can be very effective. However, therapy may not help much if your symptoms are so severe that the muscles of the hand or forearm have atrophied (shrunk).
Surgery
Surgery for TOS is usually a last resort. The surgery is directed at removing the source of compression on the nerves of the brachial plexus. The brachial plexus is the network of nerves that go to the hand and forearm. If there is an extra rib, it is usually removed. Otherwise, surgery consists of simply releasing the constricting elements and scar tissue around the nerves.
Surgery is usually done through an incision under the arm. The surgery will require a general anesthetic, which will put you to sleep. You will probably need to spend at least one night in the hospital.
Rehabilitation
What can I expect after treatment?
Nonsurgical Rehabilitation
If you are getting nonsurgical treatments, a home exercise program is essential to the treatment of TOS. This is true even if the cause of your TOS is an abnormality in the bones and muscles. You must consistently do your exercises to get the most benefit.
Usually a physical or occupational therapist will direct your exercise program. Rehabilitation may begin with a few exercises to loosen up tight muscles and joints around the compressed nerves and blood vessels. To help restore normal mobility, your therapist may prescribe stretching for the joints, muscles, and nerves. Your therapist can also help you find ways to manage your pain and avoid future problems.
You will be given exercises to strengthen the muscles of your shoulder and upper back and to stretch the muscles in the front of the chest and shoulders. Swimming can help some patients, but the backstroke and full breaststroke may worsen the condition. Your exercise program will focus on helping you sit and stand with good posture. Good posture is critical to managing TOS symptoms.
Your therapist can also give you tips to help avoid TOS pain. For example, you should limit the length of time the arms are used in outstretched or overhead positions, and don't do heavy carrying and lifting. Simple things like taking frequent breaks, changing positions, stretching, or using a hand truck or cart can bring relief. Your doctor or therapist can help you with any specific tasks that cause you pain.
After Surgery
Your rehabilitation will likely be more complex after surgery. Patients wear a sling after surgery to support the shoulder and arm. Passive movements can begin soon after surgery. But there should be no active motion for about two weeks, to allow the soft tissues time to heal.
Patients usually start doing resistive exercise and activities after three to four weeks. Therapy treatments help improve motion in the shoulder blade and arm. Posture and strengthening exercises help prevent future TOS problems.
Your surgeon and therapist will give special attention to the type of work you do. They may have suggestions to help you avoid work postures and activities that could cause problems. You'll be shown strategies to take care of any future symptoms and avoid further problems.
|