A Patient's Guide to Rheumatoid Arthritis
Rheumatoid arthritis (RA) is a chronic, or long-term, inflammatory form of arthritis. RA is considered an autoimmune disease, in which your immune system attacks the tissues of your own body. In RA, the immune system mostly attacks tissues in the joints, but it can also affect other organs of your body. In some people, RA seems to run its course more or less by itself. In others, RA gets progressively worse and leads to the destruction of joints. RA can greatly affect your ability to move and do normal tasks. RA can appear at any age, but most patients are between the ages of 30 and 50. About two million Americans have RA, and most of them are women.
This guide will help you understand
- how RA develops
- how doctors diagnose the condition
- what can be done for RA
Anatomy
Where does RA develop?
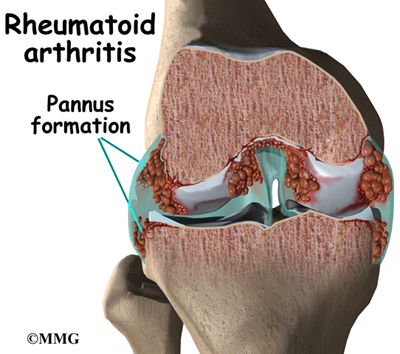
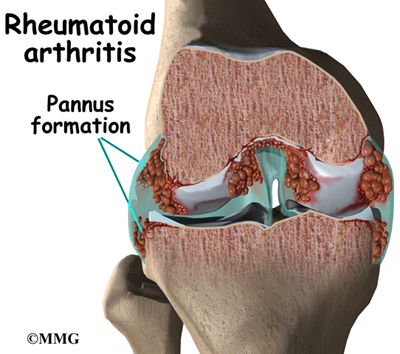
In RA, two things are happening in the joints. First, the immune system causes inflammation in the synovial membrane, called synovitis. The synovial membrane is the thin tissue that lines the inside of all joints. At first this causes extra fluid, swelling, and oozing clots in the joint. The pain and swelling of synovitis can be reversed.
Second, the synovitis itself causes other problems in the joint. The blood cells and the swollen membranes release chemicals into the synovial fluid (the lubricating fluid of the joint) that can break down or damage the tissues of the joint. This breakdown can cause permanent damage to the cartilage, bone, ligaments, and tendons inside and around the joint. The structural damage usually happens in the first to third year of the disease. The synovitis can come and go, but the structural damage progresses. As a result, the joint becomes painful and very difficult to move.
RA usually affects many corresponding joints on both sides of body. (For example, both knees, both ankles, both wrists, and the same joints in both hands may be affected.) Research indicates that almost all the joints that will be affected show symptoms of RA in the first year of the disease. This means that each joint may continue to get worse, but you probably won't have many more joints that will develop the symptoms of RA.
Most RA patients have inflammation in the tendons around the joint. (Tendons connect muscle to bone.) Nodules, or bumps, may form on the tendons, or the tendon sheath (the membrane that surrounds the tendon) may become inflamed. Inflammation can also occur in other parts of the body, like the lungs. In general, inflammation refers to symptoms of swelling, redness, heat, and pain.
Most people think of RA as a disease of the joints, but it is actually a systemic disease--it affects the whole body. That means that RA can show up in other organs, too, such as the heart, blood vessels, lungs, and eyes. Sometimes RA occurs in joints and other organs, and sometimes it occurs only in other organs. RA works somewhat differently outside the joints, but the underlying problems are still damage to the tissue and loss of function.
Causes
Why do I have this problem?
No one knows exactly what causes RA. There are probably different causes in different people. Many doctors and researchers think that a virus or bacteria might cause RA. So far studies haven't proved this. However, researchers do know that bacteria can cause swelling in the synovial membrane.
Heredity--your genes--plays a part in RA. The disease tends to run in families. If a close relative has RA, you are 16 times more likely to develop the disease yourself.
Symptoms
What does RA feel like?
The primary symptom of RA is pain in corresponding joints (both elbows, both knees, and so on). In rare cases the pain is only in one joint. Most often the pain develops over several weeks. But the pain can come on suddenly. As the pain spreads to other joints, it becomes more symmetrical, meaning that it shows up in the same places on both sides of your body. The pain is directly related to the amount of swelling in the synovial membranes. When the swelling is at its worst, your joints themselves will feel warm and swollen. The pain can come and go with the swelling.
RA patients also describe severe morning stiffness that can last up to two hours. The stiffness can be so bad that it makes it hard for you to get dressed, make breakfast, or even get out of bed. This stiffness also corresponds to the synovitis. When the synovitis goes away for a time, so does the stiffness.
About half of RA patients have rheumatoid nodules. The nodules are hard knots, from the size of a pea to the size of a golf ball, that grow under the skin in three distinct layers. They are usually found on the outside of the elbow, the Achilles tendon on your heel, the underside of your fingers, the lower abdomen, and certain toe joints. They look like the kind of bump that grows around a splinter. They don't usually hurt. Over time they tend to shrink or disappear.
Because RA is a systemic disease, most patients feel tired and weak during flare-ups. In patients who test positive for rheumatoid factor (RF) in their blood, other organ systems can also become inflamed when the joints do. About 50 percent of RA patients have systemic inflammation during joint outbreaks of RA.
Conjunctivitis, or inflammation of the eye, is common. It may be related to a disease of the eye called Sjogren's syndrome, which often occurs along with RA. The main symptom is eye dryness, but patients often can't even feel it.
RA can affect the lungs. Occasionally it can cause an inflammation of the membrane that surrounds the lungs (called the pleura), which causes pain in the side and sometimes coughing and problems breathing deeply.
RA commonly affects the nervous system, but it can be hard to tell from other symptoms of RA. Damage to the joints in the cervical spine (the neck) can eventually lead to weakness and instability between the cervical vertebrae. This damage can cause problems with the spinal cord as it travels through the neck.
Some symptoms depend on the affected joints:
- Cervical spine (the neck): Symptoms include neck stiffness, weakness, and loss of motion. Other symptoms often can't be felt or seen in exams. Ligaments are often inflamed, and there may be problems with the spinal cord or nervous system. Neck pain alone tends to get better, even when the joints are damaged. Damage to the nervous system does not usually improve.
- Shoulders: The main symptom is loss of motion. Your body's unconscious reaction to shoulder pain is simply not to use your shoulders. Since daily life doesn't require much shoulder use, frozen shoulder syndrome can set in quickly.
- Hands and wrists: Almost everyone with RA has affected wrists. Joints in the middle of your hand and fingers are usually affected. The knuckles at the ends of your fingers usually are not. RA can cause joint deformities that freeze your fingers in unusual positions. Rheumatoid nodules and tendon inflammation can make it hard to bend the fingers. Nodules can cause a locking and catching action as your fingers bend.
- Knees: It is easy to feel the swelling in the knees. A fluid-filled lump called a Baker's cyst often appears behind the knee. It can burst and leak fluid into the calf.
- Feet and ankles: RA commonly affects the joints in the middle of the toes and the ankle joints. The deformities and pain in the toes can cause problems with walking. The sole of the foot can feel tingly or numb.
The progression of RA is hard to predict. The swelling of RA flares up and dies down, and milder forms of the disease often don't require much treatment. Mild RA may even go undiagnosed.
Diagnosis
How do doctors identify RA?
No single test can confirm a diagnosis of RA. Many findings over a period of time lead to the diagnosis. In fact, your doctor can't even positively diagnose RA until you've had symptoms for at least several weeks. Early on, many characteristics of RA haven't developed yet, such as the pattern of joints that are affected, X-ray findings, and blood test changes. And RA in its early stages can look a lot like other forms of arthritis, such as lupus, psoriatic arthritis, and diseases of the spine. Your doctor will need to consider each of these diagnoses and perhaps do tests to rule them out.
Your doctor will start with a detailed health history. You will need to describe your pain and be very specific about where your pain is located and when it came on. You will also need to tell your doctor about any other medical conditions you have had and drugs you are taking. Even if these other conditions are not related to your joint pain, your doctor will need to know these things to help you find effective treatment. Your doctor will also examine your joints closely. Your doctor will be looking for bone-on-bone crepitus, a high-pitched screech that you can feel or hear in the joint. It is the sound of bone rubbing on bone, and nothing else makes this sound.
Every patient with RA has inflammation of the synovial membranes. Your doctor can confirm this by checking the count of white blood cells (WBC) in your synovial fluid. This involves inserting a thin needle into your joint and drawing out a small amount of the fluid for testing. The fluid can also be tested for other things. The WBC alone doesn't prove that you have RA. Your doctor will need to rule out other causes of synovitis.
Your doctor will also ask you to undergo a blood test. RF, or rheumatoid factor, is found in the blood of about 85 percent of RA patients. But this test alone can't confirm RA either. Some patients with RA do not have RF, and people with RF can have other forms of arthritis.
Another blood test is the erythrocyte sedimentation rate (ESR, or sed rate), which measures how fast red blood cells settle in the test tube. Red blood cells that settle faster than normal indicate inflammation in the body. But the ESR varies greatly between people. It is even possible for a patient with RA to have a normal ESR. The ESR may be more useful in monitoring the progress of your disease than in diagnosing it. A higher ESR usually means that the inflammation is more severe.
The C-reactive protein test can also monitor inflammation. It is a newer test that may be more accurate than the ESR. This test measures the amount of a certain protein that is produced by the body due to inflammation. When inflammation is very active the amount of C-reactive protein is high, and when inflammation is brought under control the level of protein decreases.
At some point your doctor will probably ask you to get X-rays of your affected joints and organs. X-rays and other imaging techniques can show damage to the cartilage and bone and the swelling in the soft tissues of the joint.
In some cases your doctor may want to biopsy the rheumatoid nodules. A small amount of the nodule is removed and examined in a laboratory.
Treatment
What can be done for the condition?
Doctors have learned much about RA in recent years, but they still don't know much more about how to truly cure the disease. They do have many strategies for treating the symptoms of RA. If you start treatment within a few months after your symptoms appear, the better you will probably do in the long-term. Early detection and treatment can help avoid the worst joint damage. Sudden remission does occur, but it's unclear how often, and it appears to be more likely within the first two years of the disease. Patients who develop RA at a young age, are RF positive, have close relatives with RA, and have RA nodules tend to have a more difficult time managing the disease.
Your doctor will prescribe one or more medications. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as aspirin and ibuprofen, can help decrease the pain and swelling. Corticosteroids taken by mouth can also help with inflammation. Because steroid use can cause other problems in your body, they are usually not be used over long periods of time, if at all possible. Corticosteroid injections into the affected joints can ease the swelling and give you immediate, short-term relief. And your doctor may prescribe eye medications, even if you have no eye symptoms. Because eye inflammation is so common with RA and is hard to diagnose, the eye drops can help prevent it from developing or becoming severe.
Disease-modifying antirheumatic drugs (DMARDs) are important in treating RA. No one is sure exactly how well DMARDs actually slow or prevent the structural damage from RA. However, tests have shown all DMARDs to be effective for at least one year of treatment.
DMARDs can be very hard on your body and can interact with other drugs, so it is not always easy to find the best medication for you. Often more than one drug is taken at the same time. Several DMARDs are frequently prescribed:
- Hydroxychloroquine is a relatively nontoxic drug that was made to treat malaria. It can be safely used with other DMARDs. It is most useful in early, mild RA. You should get regular eye check-ups while taking this drug.
- Sulfasalazine is much like hydroxychloroquine. This drug requires regular blood monitoring.
- Gold salts can cause short-term remissions. Over the long-term, however, the RA does progress. Blood and urine monitoring is required.
- Methotrexate can help manage RA, but it is unclear how much it actually changes the course of the disease. Methotrexate can be very useful over the long-term, but there are problems with flare-ups when patients stop taking it.
- Azathioprine is used with moderate and severe RA.
- Penicillamine is only used in patients who have systemic disease that doesn't respond well to other medications.
- Cyclosporine is expensive and hard on the kidneys, so it is most often used in severe RA.
- Cyclophosphamide is very effective but very toxic, so it is only used in specific cases.
- Certain antibiotics are somewhat effective in mild cases.
Combining methotrexate with another drug to get the desired results (decreased joint pain, swelling, and stiffness) is a popular and effective strategy for many patients. One group of disease modifying medications used along with methotrexate is called anti-tumor necrosis factor (TNF) agents.
Another term for the anti-TNF agents is TNF inhibitors. These are a special type of antibody also referred to as human monoclonal antibodies. They specifically target (and inhibit) tumor necrosis factor. Tumor necrosis factor (TNF) promotes the inflammatory response, which in turn causes many of the clinical problems associated with autoimmune disorders such as rheumatoid arthritis.
Anyone taking tumor necrosis inhibitors must be careful to report any signs of infection to the physician right away. There have been reports of deaths possibly associated with unrecognized or untreated infections in patients taking these immune suppressing drugs.
Symptoms of infection anywhere but commonly affecting skin, lungs, or urinary tract include fever, chills, fatigue, enlarged lymph nodes, skin rash or red streaks, cough, and/or sore throat. Upset stomach, painful urination or blood in the urine or stools are additional important symptoms that could be a signal of infection and should be reported to the physician as well.
In general, your doctor may recommend some of the following treatments that will require some effort and lifestyle changes from you:
- Patient education. RA is a frustrating and complex disease. The more you understand it, the better you can help treat your own symptoms and prevent flare-ups.
- Range-of-motion and strengthening exercises. These will most often be designed and monitored by a physical or occupational therapist.
- Equipment and gadgets, such as canes and jar openers that can help you go about your daily business without putting too much stress on affected joints.
- Gentle aerobic exercise.
- Support groups.
At least half of RA patients don't find much relief from treatment and eventually need surgery on the affected joints. Surgery, including total joint replacement, can be a very effective way to help you overcome the pain and loss of movement of RA.
For most patients, RA is a disease that comes and goes throughout their lives. But it doesn't have to be crippling. With your doctor's help, you should be able to find treatment that works for you.
|