A Patient's Guide to Pain Management: Epidural Steroid Injections
Introduction
Injections are commonly used by pain specialists, both to help diagnose the painful condition and to help treat the painful condition.
Epidural steroid injections (sometimes referred to as an ESI) are commonly used to control back and leg pain from many different causes. These injections control pain by reducing inflammation and swelling. They do not cure any of the problems they are commonly used for, but can control the symptoms for prolonged periods of time. In some cases, an epidural steroid injection may be used to control your symptoms so that you can participate more fully in a physical therapy program and become more active. Over time, maintaining an increased activity level may lead to an overall reduction in your symptoms.
This guide will help you understand
- where the injection is given
- what your doctor hopes to achieve
- what you need to do to prepare
- what might go wrong
Anatomy
What parts of the body are involved?
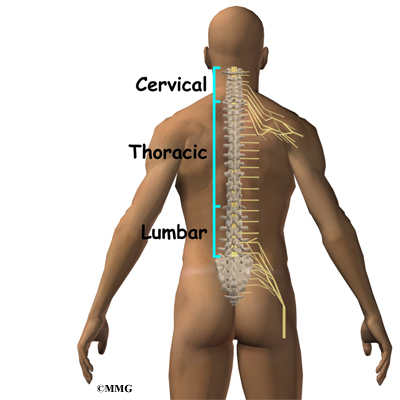
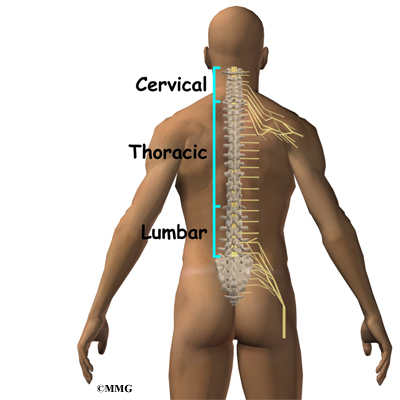
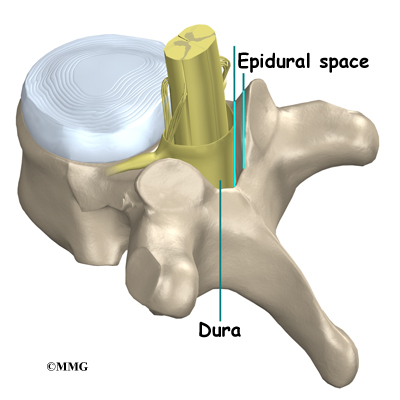
To perform an ESI, your doctor inserts a needle into the spinal canal so that the tip of the needle is in the epidural space. The epidural space is the area between the bone of the spinal canal and the covering of the spine called the dura. The dura creates a water tight sac that encloses the spinal cord and the spinal nerves. This spinal sac is filled with spinal fluid. In the cervical and thoracic spine, the spinal cord runs within the spinal canal. The spinal cord ends at the second lumbar vertebra, so in the lower lumbar spine there are only spinal nerves running within the spinal canal.
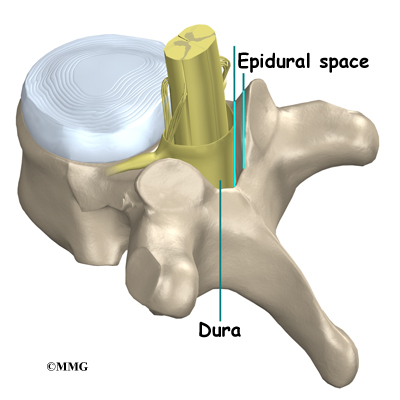
The epidural space is normally filled with fat and blood vessels. Fluid, such as the medication that is injected during an ESI, is free to flow up and down the spine and inside the epidural space to reach the spinal nerves that run inside the spinal canal.
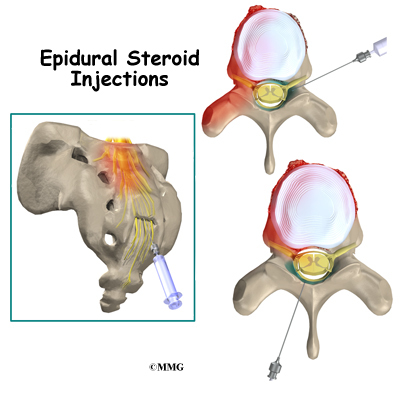
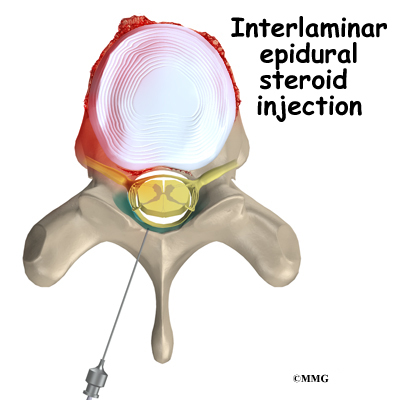
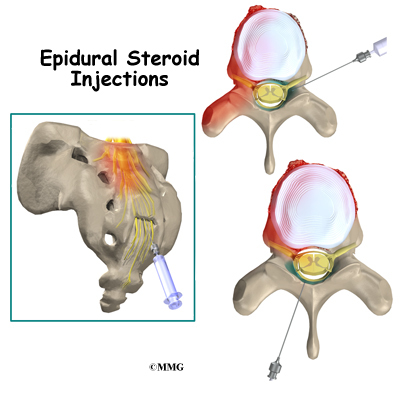
There are several openings to the spinal canal and epidural space where a needle can be placed. An ESI can be performed by placing the needle in any of these three openings. Each of these three types of ESI injections has advantages.
Related Document: A Patient's Guide to Lumbar Spine Anatomy
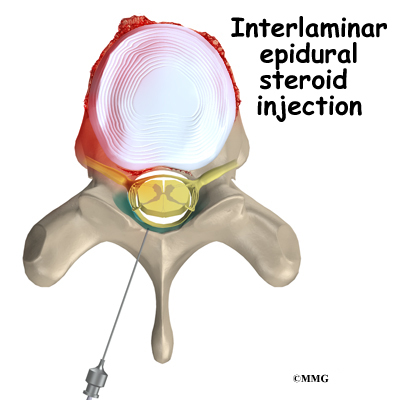
An interlaminaris performed by placing the needle directly into the spinal canal from the back of the spine between the lamina of two adjacent vertebra. The laminae are the part of the vertebrae that cover the back of the spinal canal. This type of injection places the tip of the needle in the back side of the spine. The advantage to this type of injection is that it is easy to do, even without the guidance of a fluoroscopic x-ray machine. The injection is usually done as close as possible to the area of the spine that is causing your symptoms. This puts the medications as close as possible to the problem.
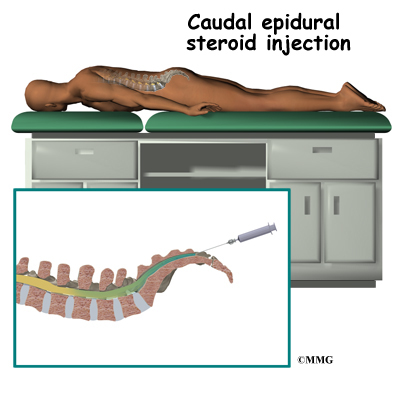
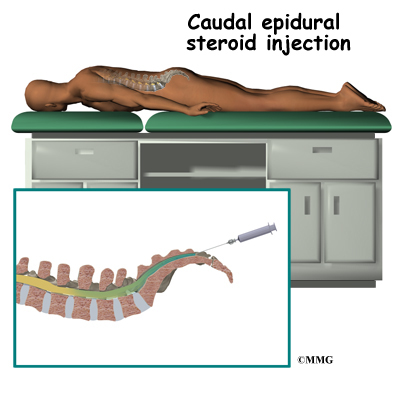
A caudal injection is also relatively easy to perform even without x-ray guidance. The caudal injection is performed at the very lower end of the spine through a small opening in the bones of the sacrum. The sacrum is made up of several vertebrae that fuse together during development to form a single large bone. The sacrum connects the pelvis to the spine. The at the tip of the sacrum leads directly to the epidural space. Fluid injected through this opening can flow upward through the epidural space and reach the nerves throughout the lower lumbar spine.
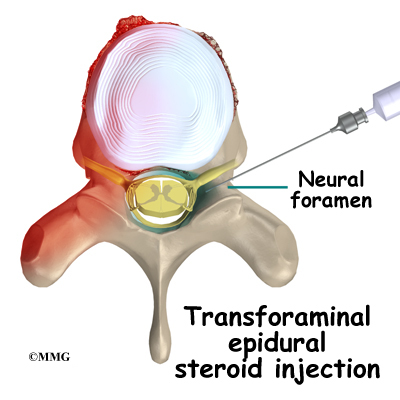
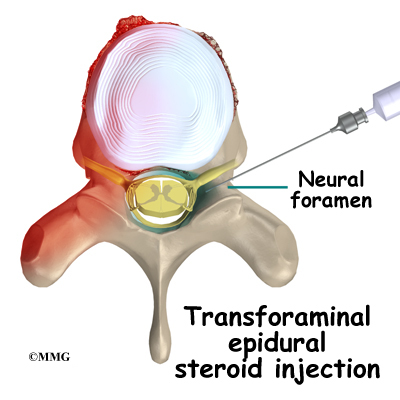
A transforaminal injection is performed by inserting the needle from the side of the spine through the neural foramen. The neural foramen is the opening where a single nerve root exits the spine. There are two neural foramen between each vertebrae, one on each side. During the transforaminal injection, your doctor places the tip of the needle into the neural foramen using the fluoroscopic x-ray machine to watch and guide the needle into the correct position. The advantage to this type of injection is that it places the medication in the front of the spinal canal, near the intervertebral disc.
Rationale
What does my physician hope to achieve?
Your doctor is recommending an ESI to try and reduce your pain. The ESI may also reduce numbness and weakness. During an ESI the medications that are normally injected include a local anesthetic and cortisone. A local anesthetic medication, such as lidocaine or bupivicaine, is the same medication that is used numb an area when you are having dental work or having a laceration sutured. The medication causes temporary numbness lasting one hour to six hours, depending on which type of anesthetic is used.
Cortisone is an extremely powerful anti-inflammatory medication. When this medication is injected around inflamed swollen nerves and connective tissues, it can reduce the inflammation and swelling. Reducing the inflammation reduces pain. Reducing swelling can allow the nerves to function better - reducing numbness and weakness. Cortisone is an extremely powerful anti-inflammatory medication. When this medication is injected around inflamed swollen nerves and connective tissues, it can reduce the inflammation and swelling. Reducing the inflammation reduces pain. Reducing swelling can allow the nerves to function better - reducing numbness and weakness.
These injections are temporary and may last from a couple of weeks to a couple of months. They may be used to reduce your symptoms so that you can more easily begin a physical therapy program with less pain. They may also be used to reduce symptoms and let the body repair the underlying condition. For example, most disc herniations cause a great deal of pain when they first happen. This is thought to be due to chemicals that leak from the torn disc and inflame the nerves. Over several weeks to months, the disc heals enough to stop leaking these chemicals. If the cortisone can reduce the symptoms at the beginning, then as the cortisone injection wears off the chemical irritation may be gone and the pain may not return. The cortisone itself does not heal the disc herniation.
In other conditions, the cortisone injection is repeated several times per year to help control the symptoms. For example, in older adults with spinal stenosis, injection therapy may be preferable to surgery. Spinal stenosis occurs when the spinal canal where the nerves travel is too tight. This results in inflammation and swelling of the nerves and soft tissues. The swelling makes the spinal canal even tighter. The nerves do not have enough room to function correctly and begin to cause pain, numbness and weakness into the legs. An ESI once every four to six months may reduce the swelling enough to reduce the pressure on the nerves and the symptoms of pain, numbness and weakness.
Preparations
How will I prepare for the procedure?
To prepare for the procedure your doctor may tell you to remain "NPO" for a certain amount of time before the procedure. This means that you should not eat or drink anything for the specified amount of time before your procedure. This means no water, no coffee, no tea - not anything. You may receive special instructions to take your usual medications with a small amount of water. Check with your doctor if you are unsure what to do.
You may be instructed to discontinue certain medications that affect the clotting of your blood several days before the injection. This reduces the risk of excessive bleeding during and after the injection. These medications may include the common Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) such as aspirin, ibuprofen, naproxen and many other medications that are commonly used to treat arthritis. If you are taking any type of blood thinning medication you should let your doctor know. You will most likely need to have this medication regulated or temporarily discontinued prior to the injection. Your doctor will need to determine if it is safe to discontinue these medications in order to have the injection.
You may need to arrange to have transportation both to and from the location where you will undergo the injection. Wear loose fitting clothing that is easy to take off and put on. You may wish to take a shower the morning of the procedure, using a bactericidal soap to reduce chances of infection. Do not wear jewelry or any type of scented oils or lotions.
Procedure
What happens during the procedure?
When you are ready to have the injection, you will be taken into the procedure area and an IV will be started. The IV allows the nurse or doctor to give you any medications that may be needed during the procedure. The IV is for your safety because it allows very rapid response if you have a problem during the procedure, such as an allergic reaction to any of the medications injected. If you are in pain or anxious, you may also be given medications through the IV for sedation during the procedure.
Most injection procedures today are done with the help of fluoroscopic guidance. The fluoroscope is an x-ray machine that allows the doctor to actually see an x-ray image while doing the procedure. This allows the doctor to watch where the needle goes as it is inserted. This makes the injection much safer and much more accurate. Once the needle is in the right location, a small amount of radiographic dye is injected. This liquid dye shows up on the x-ray image and the doctor can watch where it goes. The medication used for the injection will go in the same place, so the doctor wants to make sure that the medication will go to the right place to do the most good. Once the correct position is confirmed, the medication is injected and the needle is removed.
You will then be taken out of the procedure room to the recovery area. You will remain in the recovery area until the nurse is sure that you are stable and do not have any allergic reaction to the medications. The anesthetic may cause some temporary numbness and weakness. You will be free to go when these symptoms have resolved.
Complications
What might go wrong?
There are several complications that may occur during or after the procedure. The ESI procedure is safe and unlikely to result in a complication, but no procedure is 100% foolproof. This document doesn't provide a complete list of the possible complications, but it does highlight some of the most common problems. Complications are uncommon, but you should know what to watch for if they occur. Like most procedures where medications are injected, there is always a risk of allergic reaction.
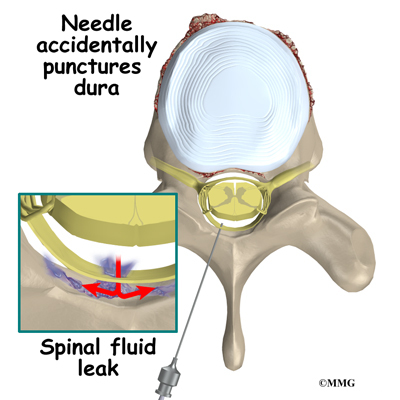
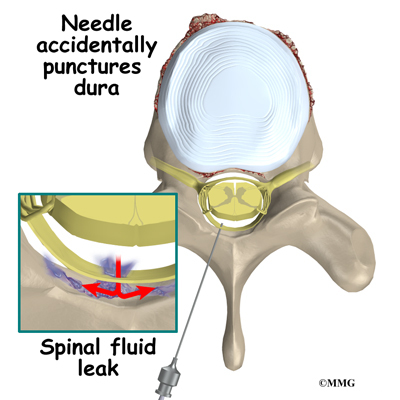
Probably the most common complication of an ESI is a wet tap. This occurs when the needle penetrates the spinal sac and enters the spinal fluid. This is the same thing that happens when your doctor performs a spinal tap or a spinal anesthetic. In itself, it is not dangerous. Because the epidural needle is larger than the spinal needle, the hole in the spinal sack may continue to leak and not seal itself off immediately. This causes a spinal fluid leak - or wet tap. This causes a very bad headache. The headache is worse when you are sitting or standing upright. It may cause nausea and vomiting. It will go away if you lie flat or with your head a bit lower than your feet. The headache occurs because the spinal fluid pressure in the skull decreases. That is why the headache goes away when you lie down - the spinal fluid pressure goes back to normal in your skull. Most spinal headaches go away in a few days when the hole in the spinal sac heals and closes. You may be instructed to stay flat for a couple of days until this occurs.
There are ways to speed up the healing of the puncture in the spinal sac. The most common treatment for a spinal headache is a blood patch. If the doctor sees that the spinal sac has been punctured before he removes the needle, this may be done at the time of the ESI. If not it may be done several days later if the headache has not gone away. This procedure involves taking a small amount of blood from a vein in your arm and injecting it into your back in the epidural space. The blood clots and patches the hole.
There are several other very rare possible complications of the ESI. These include epidural hematoma, epidural abscess and nerve damage. The epidural hematoma occurs when one of the small blood vessels around the spinal sac continues to bleed after the procedure. The bleeding can cause a large pocket of blood to form around the nerves putting too much pressure on the nerves. The epidural abscess occurs when an infection forms inside the spinal canal. The infection can cause a large pocket of pus to form around the nerves and puts too much pressure on the nerves. Both of these complications will probably require surgery to correct.
Finally, because the the injection is done inside the spinal canal, the spinal nerves can be damaged by the needle itself. This injury to the nerves will usually recover on its on and will not require any additional procedures to correct. It is rare to suffer permanent damage from this type of complication.
After Care
What happens after the procedure?
You will be able to go home soon after the procedure, probably within one hour. If all went as planned, you probably won't have any restrictions on activity or diet.
Most doctors doctors will arrange a follow-up appointment, or phone consult, within one or two weeks after the injection to see how you are doing and what effect the procedure had on your symptoms. Your doctor will be interested in how much the pain is reduced while the anesthetic (numbing medication) is working. You may be given a pain diary to record what you feel for the next several hours. This is important for making decisions, so keep track of your pain.
One question that always comes up is: How many injections are safe to have? There is no definite answer to that question. Most doctors would recommend that you limit the number of injections to three to five per year. The reason for this limit has to do with how much cortisone is safe to put in your body. Cortisone has bad side effects when you take the medication often, either as a pill or as an injection. These side effects are why doctors do not like to do these injections more often than necessary..
And remember, these injections are not a cure for your pain; they are only a part of your overall pain management plan. You will still need to continue working with the other recommendations from your pain management team.
|